INTRODUCTION
The well-known physician and author Welch1 in his book ‘Less Medicine, More Health’ states that ‘as our diagnostic technologies become more and more capable of detecting minor abnormalities in our anatomy, physiology, biochemistry and genome, so many unexpected findings increased which may not be so unexpected’. This increase in the diagnostic capacity of our techniques is accompanied by an ever-increasing use of preventive examinations in people who are not always in actual fact ill but within such a context are ‘potentially’ ill. With a well-developed rhetoric about maintaining good health and the ever use of statistics, part of the population eventually becomes ‘potentially’ ill. Meanwhile, in many cases, the data and images we get from our technical devices are not sufficiently clear in what they reflect of the complex and multifactorial phenomenon of life.
COMMENTARY
Medical practice
According to Hippocrates ‘prevention is better than cure’, but the present medical reality has little to do with the reality of the time of Hippocrates. If it was so, the Hippocratic ‘Humoral Theory’ and Hippocratic treatments such as bleeding, purging and laxatives would be utilized to treat every human disease. The main pathogen of Hippocratic medicine was considered to be the disturbance of the balance between man and his natural environment but also with his corresponding daily biotic (diet and habits)2. By improving the way of life and diet, i.e. the interaction of man with the environment in which he lives, he prevents diseases which are an expression of this bad relationship between man and his environment. The Hippocratic approach to disease was an expression of the social perceptions and practices of his time and in line with the naturalistic approaches of the prosocratics.
Since then, the view of disease, as such, has changed. Its approach today is more technical, capturing the technological orientation of modern societies as well as its integration into the dominant productive model. In this context, and in order to maintain good health and the expectation of prolonging life expectancy, preventive examinations have increased dramatically.
Eventually, when something is found, it is very difficult to stop searching further, which leads inevitably to its ‘treatment’ or ‘overtreatment’. This is where real hazards start because an unnecessary treatment can harm us. Overdiagnosis, naturally, does not only concern the cases mentioned above but includes cases such as mild hypertension, autism, menopause, osteoporosis, diabetes type II, cancer, and gene control. Concerning psychiatric diseases, we encounter the same or even greater problems, as doctors continuously add new diseases to the therapeutic range of drugs. Therefore, by definition ‘overdiagnosis occurs when individuals are diagnosed with conditions that will never cause symptoms or death’3. It could also be said that overtreatment is a side effect of the accuracy of diagnostic methods. The possibilities and accuracy of diagnostic methods have dramatically improved in recent decades and have opened new prospects in medicine. The new depiction methods along with the patient’s presentation, bring about unprecedented assurance and safety to the physician’s work (medical authority). But have we ever wondered what exactly is depicted? What does the depiction have to do with the actual functional status of the potential patient? In relation to what standards and conditions is this depiction compared to?
In modern medicine, we do not focus on a single symptom but instead perform scrutinizing exams on many other systems without any form of association between the symptom and the other systems. This is called ‘passion for diagnosis’ and is a medical phenomenon, especially among young doctors. In essence, it is the fear of not giving enough attention to something and then ‘losing’ the patient. Unfortunately, in the days of particularly increased technological capabilities in imaging and biochemical control, diagnostic passion (i.e. early diagnosis) is also transferred to those who do not have symptoms and are simply afraid they will acquire them in the future. The issues raised here are: exactly what is depicted with these technical diagnostic means; in relation to what is this imaging to be compared to; and how is this model of comparison to be defined (if any) and who and in what way to handle this model and its requirements. Passion for diagnosis gradually transforms the individual into a patient. But how many people are there who will not only undergo a treatment that will not benefit them but will also put their lives at risk?
Let us analyze a case in order to understand that medicine does not tell us the full truth. Cholesterol is the most appropriate example, probably because nowadays ‘statins’ are not simple medications but a lifestyle. In the eighth edition of Harrison’s pathology in 1977 (the golden bible of medicine), the normal limit of cholesterol was 300 mg/dL and only those who surpassed it had to take medication. Gradually, by adding risk factors (hypertension, smoking, coronary artery disease), with the separation of cholesterol to good and bad, with the plethora of investigations and the opinions of specialists, the normal boundary of cholesterol fell to 200 mg/dL. Can you comprehend what exactly the reduction of the cholesterol threshold from 240 to 200 mg/dL meant? It meant that 42 million Americans were added as potential customers4. The big winners became the pharmaceutical companies. Lipitor alone (most known statin), has an annual turnover for Pfizer of 15 billion US$, making it the most successful abused formulation of all time5.
The way in which the science is exercised in the field of biotechnology and by pharmaceutical companies in the last two to three decades is as close as possible to what we call Big Science6. Large funding involving state governments and big politics, where the protection of corporate and national interests appear as strategies, is Big Science. Moreover, if we acknowledge the expanded collaborations of many scientists, techniques and staff as well as the interconnection of facilities around the world as a network of cooperation, information exchange and new knowledge production in the pharmaceutical field, then the formal definition of Big Science is completed with major partnerships and infrastructure.
Nevertheless, specialized doctors will argue that we are unfair since people gain in health. But experts also make mistakes, deliberately or not. Let us look at ‘the Gulf of Statistics’ through the Classical Work of 1998 that changed many things in the treatment of cholesterol7. Until 1998, the limit of normal cholesterol was 240 mg/dL. However, the study, with the prestige of the most reliable medical methodology (i.e. randomization, which is also disputed)8, found that those who had cholesterol ranging from 228 to 184 mg/dL had less risk for acute coronary episode. In fact, in the five-year period, 5% of patients who did not receive statins had a cardiac episode against 3% of the statin patients. Indeed, there was a 40% reduction in coronary episodes for those taking statins. But this is half the truth. The other half is as follows: the benefit is only 2% (5% - 3% = 2%), meaning that out of 100 patients taking statins, only two will benefit and 98 will not9. Also, we should think about the risks of the side effects of drugs, lost time of prescribing, cost, etc.
A doctor on the other hand, in fear of misdiagnosis, or because of financial transactions with a pharmaceutical company would recommend the medication. Still, he would not be considered a good physician, because he delivered only half the truth. In addition, the contrivance of statistics is easily transferred to the general public through journalists or ‘specialists’ who explain to the public whether this drug or the other, or which treatment, reduces by about 40% the complications or improves health. Of course, they will not mention anything about the plethora of people who have to undergo treatment in order for one patient to benefit (‘Number Needed to Treat’)1.
What is ultimately crucial to understand is that high total cholesterol is not a ‘medical condition’ that needs treatment but a single risk factor among many others that increases the chances of heart disease or stroke. After all, the phenomenon of life – and the issue of health that falls within the phenomenon of life – is multifactorial and multilevel; it does not seem to be characterized by immediate and direct causal connections but rather by corresponding probabilistic dynamics.
Overdiagnosis in medicine
We do not accept that all modern medicine is good. On the contrary, we believe that, if we are not attentive, medicine can hurt us. Today, independent scientists and researchers highlight the huge issue of overdiagnosis that began to hit societies since the 1970s as a silent pandemic. Overdiagnosis, as part of the general ‘medicalization’ of life, targets healthy, asymptomatic people, where in the pretext of potential risks (which inevitably will happen at some point in the future), undergo medical examinations. Diagnostic examinations, in turn lead to interventions that usually cure something that would never cause symptoms or death. Today we know that 60% of men over 80 years old have prostate cancer but will die from another cause1. Today we know that in the West the rates of thyroid cancer, melanoma and breast cancer have increased, while deaths from these cancers remained relatively stable compared to 197510. Table 1 compares the rate of incidence for breast cancer in women and prostate cancer in men.
Figure 1
Rate of incidence for breast cancer in women and prostate cancer in men11 (with permission from the authors)
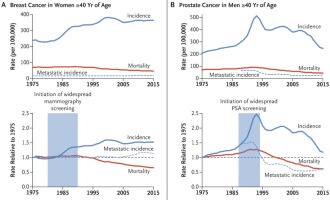
In the top charts, one can see that there was an increase in incidence and a small reduction in cancer related deaths (mortality). While in the lower graphs, it can be seen that the increase in diagnosis coincides with the spread of mammography and prostate antigen (PSA) test (colored area). The phenomenon can be explained in two ways: either there was a true increase in cancers or there was an overdiagnosis. However, the stability of metastatic breast cancer justifies overdiagnosis. But how would doctors in favor of early diagnosis explain this fact? They would say that there is a true growth in cancer rates and that improvements in diagnosis and treatment are such that they stabilized the number of deaths. Although it seems a reasonable assumption, it is however equivocal because of two parameters needing to be explained (increased cancer cases and improving medical care) instead of one (overdiagnosis).
In fact, we do not have a true increase in cancer cases but overdiagnosis. The same pattern is repeated in almost all cancers. The increase in new cancer diagnoses is due to better and more accurate screening (i.e. advanced biotechnology), defence medicine, and our improved financial capabilities. It is also due to the fact that we ask for more care through examinations and ultimately to our fear of tomorrow. But if we think that for about 65 years of our life, we will be healthy (Healthy Life Years – Eurostat), which accounts for about 81% of life expectancy, then we have no reason to be afraid, or run to doctors, diagnostic centers and hospitals without having signs or symptoms. If we have symptoms, normally, we will also have a problem – that is common sense. If doctors insist that we need to do preventive/diagnostic tests they should explain the risks and complications of a preventive/diagnostic test (screening test). If doctors do not inform patients correctly and methodically about the problems of overdiagnosis, then, there may be room to disagree and there may be a need for criticism; at the same time it seems logical that society is turning to alternative medicine and increasing all kinds of negativity and skepticism. Society’s trust in the medical community is being shaken. The credibility of science is being burgled. Is ‘less medicine, more health’1? It seems to be going there, even though the pharmaceutical companies (with 500 billion US$ turn over per year) are fighting a hard battle to weaken our role, that is, to have less power.
CONCLUSION
Real medicine, good medicine, is that of ‘medicine of signs and symptoms’ and of child vaccination, not ‘laboratory medicine’ (namely clinical medicine – emergency or scheduled). Yet this medicine is not as lucrative as ‘bad medicine’, that is, blind diagnostic medical medicine without symptoms, medicines that only heal numbers above thresholds, interventions that are promoted by the companies that sell the robots and machinery that materialize them, i.e. medicine of ‘fear and profit’. Nowadays, lucrative is medicine that sells health as a product, or to be precise, sells normal body debilitation, which will inevitably come with time. It sells normal debilitation, after it first ‘defines’ it as a disease. So, this medicine only cares about profit and not the jobs it offers and its contribution to reducing unemployment rate, no matter how often pharmaceutical and biotechnology companies use this argument. Improving society’s health and decreasing unemployment are two different objectives and they should be treated in different ways using diverse interventions. The purpose of commercial development does not sanctify the means of pharmaceutical formulations or medical machines, like a ‘home oximeter’.
Of course, we should not avoid doctors when sick. The problem of overdiagnosis begins with ‘what we do when we are healthy’ and to what extend do we have to look for things that can pose risks. Does the search for a hidden disease place us in greater risk since many ‘diseases’ are not intended to harm us? Should the doctrine of early diagnosis (without support from the medical history and the symptoms) be revised since it has long been known that medical history offers 50% of the diagnosis while the routine examinations just 1%12? Should the blind game of probabilities, that is, the game of early diagnosis, be replaced with what we can actively do, such as stopping bad habits (e.g. stop smoking) and engage in better nutrition, start exercising, maintain normal weight, or avoiding risky behavior (speeding when driving) etc.? In our opinion, the biggest problem of modern medicine with philosophical, scientific, individual (mental), social, ethical, legal and economic ramifications is overdiagnosis.


